48 yo male transfer from an OSH with the diagnosis of a DVT. The patient had no past medical history and was experiencing leg pain after a 5 hour plane ride and subsequently was found to have an elevated d-dimer, no further imaging was obtained prior to the patient being transferred. The patient did report some shortness of breath, so an ultrasound was used to look for evidence of right heart strain (RHS), and the following images were obtained. What is the diagnosis?

Answer: Complete aortic dissection.
Due to the transfer diagnosis of DVT and the patient reporting mild shortness of breath, a bedside ultrasound was performed to look for any evidence of right heart strain. Although no 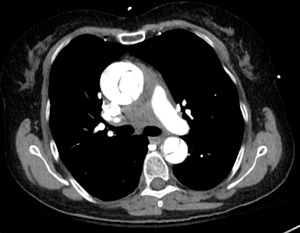 right heart strain was appreciated, it was noted that the patient had a dilated aortic root. This prompted further evaluation of the aorta, which uncovered an aortic intimal flap, confirming the diagnosis of an aortic dissection. CT surgery was called, and while they were arriving in the hospital, the patient’s blood pressure dropped to the 50’s systolic. Blood was given and the patients BP stabilized. CT scan confirmed the diagnosis, and the patient was taken to the OR, where he received an aortic graft and left the hospital some days later without major complication.
right heart strain was appreciated, it was noted that the patient had a dilated aortic root. This prompted further evaluation of the aorta, which uncovered an aortic intimal flap, confirming the diagnosis of an aortic dissection. CT surgery was called, and while they were arriving in the hospital, the patient’s blood pressure dropped to the 50’s systolic. Blood was given and the patients BP stabilized. CT scan confirmed the diagnosis, and the patient was taken to the OR, where he received an aortic graft and left the hospital some days later without major complication.
- Aortic dissections form when shearing intravascular forces cause the intima and media of the aortic wall to separate.1
- While many cases are idiopathic, the most common identifiable risk factors are hypertension, turner syndrome and bicuspid aortic valve.1
- The mortality associated for aortic dissection involving the ascending aorta has been reported to be between 29-45%.1 Some sources state that the mortality increases by 1-2% an hour, 2 making early diagnosis an important predictor of survival.
- While many patients present with the classic tearing chest pain that radiates to the back, up to 15% of patients can present with no reports of pain.2
- D-dimer has been reported to be a good test for ruling out aortic dissection. In a relatively recent meta analysis, d-dimer was found to have 97% sensitivity for ruling out AD, but was reported to have a specificity of 56%,3 which makes it a poor test for ruling
 in AD.
in AD. - The evaluation of the aorta for AD involves two locations: The thorax and the abdomen.
- In the abdomen, a curvilinear probe is placed in the midline, starting in the epigastrium. The aorta should be visualized anterior to the spine, and lateral to the IVC. If a dissection flap is visualized inside the aorta, be highly suspicious for AD.

- In the thorax, the first place to look is by using the parasternal long axis view of the heart, focusing on the aortic outflow tract and the aorta. Any intimal flap here essentially confirms an AD.

- A suprasternal view can also be helpful in the confirmation of an AD.
- Rosenberg H, Al-Rajhi K. ED ultrasound diagnosis of a type B aortic dissection using the suprasternal view. Am J Emerg Med. 2012;30:(9)2084.e1-5. [pubmed]
- Fojtik JP, Costantino TG, Dean AJ. The diagnosis of aortic dissection by emergency medicine ultrasound. J Emerg Med. 2007;32:(2)191-6. [pubmed]
- Shimony A, Filion KB, Mottillo S, Dourian T, Eisenberg MJ. Meta-analysis of usefulness of d-dimer to diagnose acute aortic dissection. Am J Cardiol. 2011;107:(8)1227-34. [pubmed]




