This patient is a 61 year old female with a history of hypertension and diabetes who presents with 3 weeks of intermittent exertional left sided chest pain. The pain is dull, non-pleuritic, always comes on when walking around and resolves with rest. +shortness of breath. Vitals: 95/50 125 22 98.6 97% RA. What diagnosis is suggested by the following bedside echo, and what can be measured to clinch the diagnosis?


Answer: Pulmonary Embolism, a 60/60 sign would clinch the diagnosis
The initial presentation was strongly suggestive of coronary ischemia. The ECG performed demonstrates inverted anterior T-waves and ST depression. There are flattened/inverted T-waves in the inferior leads as well. Initial impression was that of a anterior ischemia, but posterior STEMI was also a consideration. Inverted anterior and inferior T-waves should prompt the clinician to consider a large pulmonary embolism (PE) with right ventricular (RV) strain.
This bedside echocardiogram demonstrates a dilated right ventricle, with a RV:LV ratio greater than one and a McConnell Sign on the apical view. The intraventricular and intra-atrial septa appear to bow into the left heart, suggesting high right sided pressures. The parasternal short axis view demonstrates a D-shaped left ventricle. The parasternal long view shows a normal left ventricular ejection fraction.
- When assessing a bedside echo for signs of PE, it is important to consider a chronic cause of RV dysfunction. Signs of chronic RV dysfunction are RVH and very high pulmonary systolic pressures, discussed further here. A McConnell Sign has been found to be nonspecific for pulmonary embolism.1,2,3
- Bedside echo will be completely normal in most cases of PE. This is becoming more and more common, as CTPA utilization increases and small low risk clots are identified.
- However, when a patient presents with a submassive or larger pulmonary embolism, by definition RV dysfunction will be present on the echo. Our patient presented with a shock index greater than 1 (HR/SBP), suggesting a potentially large clot.
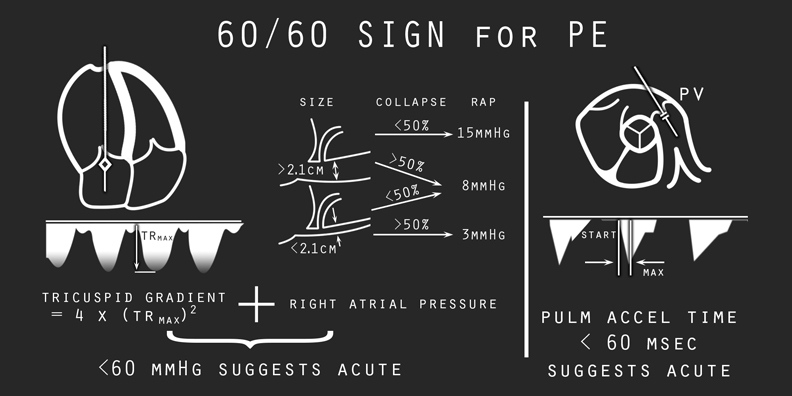
- One echo finding that has been found to be 94% specific for PE is the so called 60/60 sign. This refers to an RV systolic pressure (RVSP) less than 60 mmHg and a pulmonary acceleration time (PAT) less than 60 msec.4
- A very high RVSP often can only be generated in the setting of chronic pulmonary hypertension, so it makes sense that an RVSP < 60 mmHg suggests an acute problem.
- To measure RVSP, the sonographer must first identify a tricuspid regurgitation (TR) jet on an apical view using color doppler. Color is required to find the jet, which is often eccentric. An improved color doppler
 frame rate can be obtained by creating a small echo wedge, and by sizing the color window to be only as large as it needs to be to visualize the jet. Next, a continuous wave doppler spike should be placed in the path of the jet, and the peak should be measured. The modified bernoulli equation is then used to calculate the tricuspid gradient (TG) (calculator here). The final part of the RVSP equation is the right atrial pressure (RAP). RVSP = TG + RAP. RAP is estimated at 3, 8, 15 mmHg by viewing the IVC in the spontaneously breathing patient. RVSP < 60 is suggestive of an acute pulmonary hypertension (PH). Do note, however, that normal subjects will have a RVSP < 60 mmHg. This sign should only be applied to patients with signs of RV strain and significant PH, typically RVSP >40 mmHg.5
frame rate can be obtained by creating a small echo wedge, and by sizing the color window to be only as large as it needs to be to visualize the jet. Next, a continuous wave doppler spike should be placed in the path of the jet, and the peak should be measured. The modified bernoulli equation is then used to calculate the tricuspid gradient (TG) (calculator here). The final part of the RVSP equation is the right atrial pressure (RAP). RVSP = TG + RAP. RAP is estimated at 3, 8, 15 mmHg by viewing the IVC in the spontaneously breathing patient. RVSP < 60 is suggestive of an acute pulmonary hypertension (PH). Do note, however, that normal subjects will have a RVSP < 60 mmHg. This sign should only be applied to patients with signs of RV strain and significant PH, typically RVSP >40 mmHg.5 - PAT refers to the amount of time it takes for the pulmonic velocity to peak. A distal, chronic pulmonary arterial problem would result in a longer PAT as the summative compliance of the pulmonary vasculature accepts the RV output more slowly before it peaks: imagine blowing up a large balloon. Alternately, a proximal occlusion (PE) causes the velocity to peak quickly with little vascular compliance: imagine blowing through an occluded straw.
- To measure the PAT: first obtain a typical parasternal short axis view at the level of the mitral valve, then slide up toward the base of the heart until you see the aortic valve (Mercedes Benz symbol) in the shot.
 From this view you should be able to visualize the RV outflow tract and pulmonic valve (PV). Place a pulse wave (PW) spike through the valve and the hit the PW button on your machine. Below the x-axis you will see a blood flow velocity through the PV. To calculate the PAT, simply measure the time from the beginning of the blood flow to the peak. Increasing the
From this view you should be able to visualize the RV outflow tract and pulmonic valve (PV). Place a pulse wave (PW) spike through the valve and the hit the PW button on your machine. Below the x-axis you will see a blood flow velocity through the PV. To calculate the PAT, simply measure the time from the beginning of the blood flow to the peak. Increasing the  sweep speed will allow a more accurate measurement of the PAT, and this is key since we are dealing with very short times. Be sure to include any velocity spike due to the PV itself in your measurement. Precise angulation of the PW gate along the axis of flow is not necessary, as we are measuring the time to peak and not the peak itself. PAT < 60 msec suggests an acute cause of the PH as the velocity and pressure peak very quickly.
sweep speed will allow a more accurate measurement of the PAT, and this is key since we are dealing with very short times. Be sure to include any velocity spike due to the PV itself in your measurement. Precise angulation of the PW gate along the axis of flow is not necessary, as we are measuring the time to peak and not the peak itself. PAT < 60 msec suggests an acute cause of the PH as the velocity and pressure peak very quickly.
Our patient had a measured RVSP of 58 and a PAT of 31 msec, a positive 60/60 sign. This prompted a PE evaluation rather than a cardiology consult. Her creatinine was noted to be 1.9, precluding a CTPA, so a VQ Scan was performed. VQ scan showed a high probability (>80%) of pulmonary embolism. The patient’s shock index improved with a small fluid bolus and he was started on a heparin gtt.
- McConnell MV, Solomon SD, Rayan ME, Come PC, Goldhaber SZ, Lee RT. Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism. The American journal of cardiology. 78(4):469-73. 1996. [pubmed]
- Casazza F, Bongarzoni A, Capozi A, Agostoni O. Regional right ventricular dysfunction in acute pulmonary embolism and right ventricular infarction. Eur J Echocardiogr. 2005;6(1):11-4. [PDF]
- López-Candales A, Edelman K. Right ventricular outflow tract systolic excursion: a distinguishing echocardiographic finding in acute pulmonary embolism. Echocardiography (Mount Kisco, N.Y.). 30(6):649-57. 2013. [pubmed]
- Kurzyna M, Torbicki A, Pruszczyk P. Disturbed right ventricular ejection pattern as a new Doppler echocardiographic sign of acute pulmonary embolism. The American journal of cardiology. 90(5):507-11. 2002. [pubmed]
- Armstrong DW, Tsimiklis G, Matangi MF. Factors influencing the echocardiographic estimate of right ventricular systolic pressure in normal patients and clinically relevant ranges according to age. The Canadian Journal of Cardiology. 2010;26(2):e35-e39. [PDF]



