Diagnosis: Ruptured Heterotopic Pregnancy
This patient presents with a heterotopic pregnancy (HP): that is, an intrauterine pregnancy plus a concurrent ectopic pregnancy. She was currently undergoing fertility treatment and had been taking clomiphene (Clomid®) to induce ovulation.
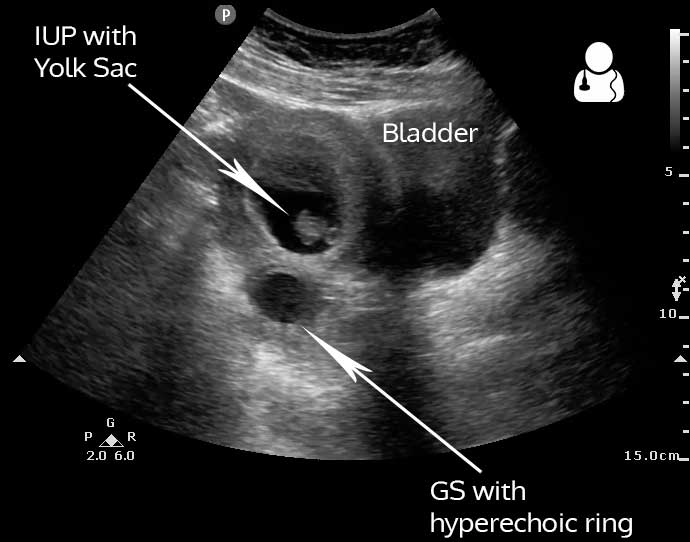
The findings on this scan that suggest heterotopic pregnancy are the intrauterine pregnancy (IUP) and empty extrauterine gestational sac seen as a hyperechoic ring posterior-lateral to the uterus. The free fluid in the right upper quadrant is identified by the hypoechoic stripe in Morison’s Pouch, suggesting a ruptured HP.
- Spontaneous heterotopic pregnancy without fertility treatment is rare, with an estimated incidence of 1/20,000. This allows the sonographer to essentially rule out ectopic pregnancy if a clear IUP is identified.
- Clomid increases the risk of HP to 1/900, while in-vitro fertilization dramatically increases the risk to ~1/100 or higher depending on the number of transferred embryos.1,2 Other fertility treatments have been associated with HP, including Gamete and Zygote Intrafallopian Tube Transfer (GIFT/ZIFT).3
- Patients who are undergoing fertility treatment and present with signs or symptoms of ectopic pregnancy should be considered to have a HP until proven otherwise.
- Transvaginal ultrasound has been shown to be 92% sensitive and 100% specific for the detection of HP in a recent study.4 This is quite similar to the sensitivity for a typical ectopic pregnancy.
- Ultrasound findings suggestive of HP are an intrauterine gestational sac plus “(1) an inhomogeneous adnexal mass; (2) an empty extrauterine gestational sac seen as a hyperechoic ring; or (3) a yolk sac and/or fetal pole with or without cardiac activity in an extrauterine sac.”4
- The adnexa should be carefully visualized in all pregnant patients, even if an IUP is identified.
- It is common for there to be discordance in visibility of fetal cardiac activity between the IUP and ectopic pregnancy.
- Bello GV, Schonholz D, Moshirpur J, Jeng DY, Berkowitz RL. Combined pregnancy: the Mount Sinai experience. Obstet Gynecol Surv. 1986;41(10):603-13. [pubmed]
- Dor J, Seidman DS, Levran D, Ben-rafael Z, Ben-shlomo I, Mashiach S. The incidence of combined intrauterine and extrauterine pregnancy after in vitro fertilization and embryo transfer. Fertil Steril. 1991;55(4):833-4. [pubmed]
- Wang YL, Yang TS, Chang SP, Ng HT. Heterotopic pregnancy after GIFT managed with expectancy: a case report. Zhonghua Yi Xue Za Zhi (Taipei). 1996;58(3):218-22. [pubmed]
- Li XH, Ouyang Y, Lu GX. Value of transvaginal sonography in diagnosing heterotopic pregnancy after in-vitro fertilization with embryo transfer. Ultrasound Obstet Gynecol. 2013;41(5):563-9. [pubmed]
- Condous G, Okaro E, Khalid A, et al. The accuracy of transvaginal ultrasonography for the diagnosis of ectopic pregnancy prior to surgery. Hum Reprod. 2005;20(5):1404-9. [pubmed]



