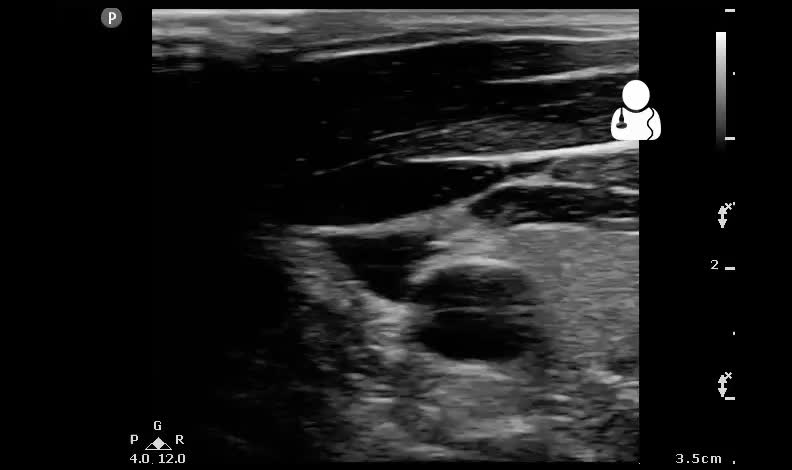
This is a critically ill 59 year old diabetic male who presents with severe altered mental status and a fever of 103.4F. You intubate the patient upon arrival because he does not appear to be protecting his airway. Vitals show a systolic blood pressure of 60/40. You obtain the following ultrasound of the neck vessels. What does the patient need based on this scan?

Answer: IV Fluids
This scan of the neck demonstrate a completely collapsing internal jugular (IJ) vein. The carotid artery is normal caliber and shows no evidence of dissection flap or aneurysm. The suspected cause of this patient’s hypotension was severe sepsis and volume depletion. It is important to know how much fluid to provide your septic patient. Gone are the days of blindly giving 2 Liters of crystalloid, then switching over to pressors and maintenance fluids if hypotension continues.
- In the spontaneously breathing patient, the pressure in the central venous circulation (CVP) decreases with each inspiration (often seen and described as IVC collapse). An IVC that collapses > 50% has been shown to correlate with a low CVP.1 Taken within the patient’s clinical context, this can be a useful piece of clinical data, but does not predict volume responsiveness (VR) with certainty.
- In the ventilated patient, the physiology flips. A positive pressure breath results in an increase in the central venous pressure, causing distension of the central veins. Looking at the IVC, a distensibility index ([IVCmax-IVCmin]/IVCmin) has been shown to correlate not with CVP, but with actual volume responsiveness. An IVC DI > 18% predicts volume responsiveness with a 90% sensitivity and specificity.2,3
- Recently, there has been an interest in looking at the IJ DI as a predictor of VR. There are several advantages to looking at the IJ over the IVC: the IJ is almost always able to be imaged and it lends itself well to m-mode for accurate measurement. M-mode measurement of the IVC is unpredictable because of the cranial-caudal respiratory phasic movement of the the IVC:
- Interestingly, the IJ DI value that is predictive of volume responsiveness is exactly the same as in the IVC. IJ DI ([IJmax-IJmin]/IJmin) > 18% means that the patient’s stroke volume will go up with an IV fluid bolus with a 80% sensitivity and an 85% specificity. One important caveat in this study was that it did exclude patients with a known history of cardiovascular disease.4
- There are many other ways to predict volume responsiveness: pulse pressure variation, VTI variation, VTI direct stroke volume estimation with a straight leg raise or bolus, and thoracic impedance cardiography.5
- Technically, this patient’s IJ DI can be measured with m-mode, and the following image obtained:
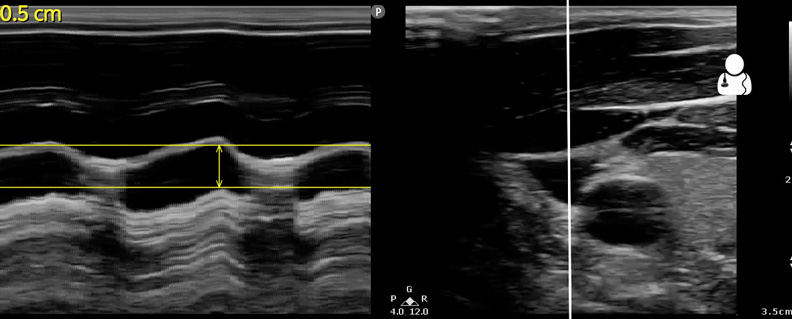
- So, for our patient IJ DI = 0.5/0 = ∞. Although here, it’s easy to just eyeball this complete collapse without measuring anything.
- Along with pressors and timely antibiotics, this patient received several LR boluses with serial IJ measurements until his IJ DI dropped below 18%. Following this resuscitation, the patient was transferred to the ICU and eventually survived this infection.
- Brennan JM, Blair JE, Goonewardena S. Reappraisal of the use of inferior vena cava for estimating right atrial pressure. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 20(7):857-61. 2007. [pubmed]
- Barbier C, Loubières Y, Schmit C. Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive care medicine. 30(9):1740-6. 2004. [pubmed]
- Feissel M, Michard F, Faller JP, Teboul JL. The respiratory variation in inferior vena cava diameter as a guide to fluid therapy. Intensive care medicine. 30(9):1834-7. 2004. [pubmed]
- Guarracino F, Ferro B, Forfori F, Bertini P, Magliacano L, Pinsky MR. Jugular vein distensibility predicts fluid responsiveness in septic patients. Critical care (London, England). 18(6):647. 2014. [pubmed]
- Marik PE, Monnet X, Teboul JL. Hemodynamic parameters to guide fluid therapy. Annals of intensive care. 1(1):1. 2011. [PDF]